Beekman carefully holds out a Petri dish. In it are two ultrathin chips barely two centimetres wide. No, a photo is out of the question; experts would be able to get information from it, which is not the intention. This chip, the latest product to emerge from Beekman’s start-up ECsens, is still a secret. But the sensor is capable of unprecedented things, says Beekman.
The chip, a nanosensor, can detect tumour vesicles in the bloodstream, in principle with 100 per cent accuracy. In other words, it never misses a thing. It is looking for what the medical literature calls tumour-derived extracellular vesicles(tdEVs). Body cells are constantly secreting tiny sacs containing nucleic acids, for example, or proteins. They are a bit like parcels that cells use to communicate with one another.
Sensitive
Beekman uses those vesicles to detect the presence of cancer cells. That is possible because the surfaces of tumour vesicles contain a protein (epCAM) that is specific for cells that are not normally found in the blood. That makes them good markers for cancer. The sensor uses that protein to differentiate between tumour vesicles and vesicles secreted by other cells. And it turns out to have unprecedented sensitivity.
‘Single-vesicle detection is a world first,’ Beekman concludes confidently. ‘The data is less than a week old.’ The chip that he shows is the follow-up to an earlier version that was announced last month by the University of Twente. Beekman works closely with his colleague at Twente and ECsens co-founder, Dilu Mathew. Twente is responsible for the sensor technology, Wageningen for the chemistry. That first nanosensor had a lower limit of detection (LLD) of 10 tumour vesicles per microlitre (millionth of a litre) of blood.
Beekman and Mathew’s announcement of that biosensor made the cover of Nano Letters, a leading journal published by the American Chemical Society. ‘We’re very proud of that,’ says the PhD candidate. ‘But that sensitivity is not good enough for proper detection. The sensor needs to be at least 100 times more sensitive.’ Which they have now managed. So fast? Beekman: ‘The article in Nano Letters was based on data collected 18 months ago. We have been working further since then.’

Nanolab on a chip
First, a bit more on how the sensor works. It uses antibodies and electrochemistry. The antibodies make sure that tumour vesicles are selectively detected. An enzyme attached to the antibody then causes an electrical signal to be produced that can be measured. Beekman does not want to disclose much about the improvements they have made. ‘We used electrochemistry to make sure the tumour particles gravitate spontaneously towards the detector. That is why you don’t miss them anymore.’
The sensor is essentially a nanolab on a chip. The vesicles themselves are less than 100 nanometres across. The electrodes that detect the signal are spaced 120 nanometres apart. ‘If you stare at your thumbnail for one minute, it will have grown 100 nanometres’: this is Beekman’s favourite comparison to show how high-tech the method is. A patent application has been submitted for the technique.
Last autumn, Beekman and Mathew won the 4TU Impact Challenge. That award will take the researchers and their company to the World Expo in Dubai early next year. In the meantime, they already have a quarter of a million euros in grants to perfect the sensor. That means testing it with real blood rather than material from cultivated cell lines. ‘The question is whether we can improve the chemistry so that it also works in blood plasma. Plasma contains a lot of biomaterials that could disturb the signal.’
The question is whether we can improve the chemistry so that it also works in blood plasma
Pepijn Beekman

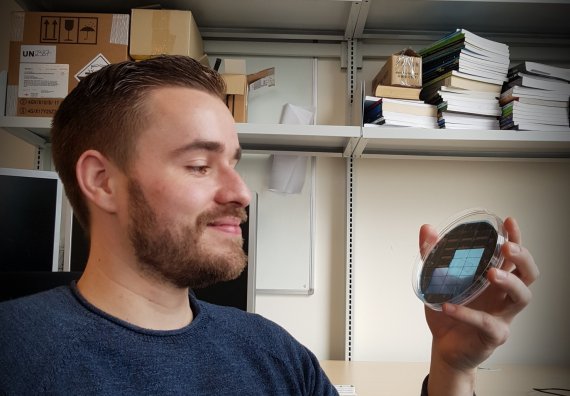 Photo: Roelof Kleis
Photo: Roelof Kleis